Results of the Minnesota Psychological Association Survey on the Use of Electronic Health Records
Effective January 1, 2015, Minnesota law required that all healthcare providers in the state adopt and use an interoperable electronic health record system (EHR). This deadline brought with it controversy among behavioral health providers, many of whom began to advocate for repealing the Minnesota EHR Mandate. Concerns expressed and shared by many psychologists and other behavioral healthcare providers seemed to converge on issues related to patient privacy and security, costs of EHR adoption particularly for small businesses, and the absence of a choice of whether or not to use EHR. Dr. Stephen Huey, a Minnesota psychologist, broadly distributed a 25-page document (Huey, 2014) outlining these concerns. This white paper generated support among psychologists toward repealing the EHR Mandate. Subsequently, Dr. Richard Sethre, another Minnesota psychologist, created and distributed what he described to be an informal survey of behavioral health providers that yielded responses from 567 of the 3783 Licensed Psychologists in Minnesota (Sethre, 2015).
In response to calls from members of the Minnesota Psychological Association (MPA) for a formal position statement on the MN EHR Mandate, the leadership of MPA organized a panel of speakers for the annual convention on the EHR Mandate topic with representatives on both sides of the controversy. The panel, moderated by Dr. Robin McLeod, President-Elect of MPA, included five speakers: Dr. Stephen Huey; Dr. Trisha Stark, chair of the MPA legislative committee and EHR Task Force; Dr. Lee Beecher, a prominent psychiatrist and strong advocate for patient rights; and, Karen Soderberg and Bob Johnson, both from the Department of Health Information Technology at the Minnesota Department of Health. An hour of the convention break-out session EHR panel was devoted to an open microphone exchange allowing comments and questions from psychologists in attendance, with members of the MPA leadership present to listen to and take in what members were saying.
Prior to the convention, MPA leadership designed and distributed a survey of the MPA membership on the topic of the MN EHR Mandate in an attempt to learn more about the attitudes of members. Because the Sethre survey was informal and did not collect data on the professional association membership status of respondents, the MPA EHR Mandate Survey was addressed to MPA members only. The hope was that by listening to members, both at the annual convention and through results of the survey, the MPA Governing Council would convene to develop a formal position statement that would best reflect opinions and attitudes of its members. Preliminary results of the survey were presented at the annual convention (McLeod, 2015). This paper is hereby submitted to deliver the more detailed report of the survey results as promised at the convention.
Methodology
Item development
The survey was designed to assess demographic characteristics of respondents, and to elicit detailed attitudes about EHR. The language used in the attitude measure was crafted to maintain close fidelity to the various positions and arguments that are being expressed by psychologists in Minnesota as well as across the country. Therefore, a number of sources were used in item development including (1) Arguments presented in the Huey document referenced above, (2) discussions on MPA listservs, and (3) a brief review of articles on the topic of EHR in behavioral healthcare settings. Several drafts of items were distributed among Minnesota psychologists to fine-tune phrasing for clarity. In order to avoid the appearance of bias in the survey, attention also was given to phrasing items so that an equal number of items were phrased in support of and in opposition to the use of EHR.
The final draft of the survey contained four main sections. First, demographic data was gathered followed by information about respondents’ comfort and familiarity with computers and EHR systems. Next, global ratings were elicited to indicate general approval or disapproval of the use of EHR, and finally, a 19-item Likert-type scale was presented to measure attitudes about EHR based on a wide range of specific factors (EHR Attitude Scale). There also were six open-response items that allowed respondents to write in more detail about their concerns regarding EHR and the Minnesota EHR mandate.
Survey Administration and Response
A link to the MPA MN EHR Mandate survey was sent in an email blast to all members of the Minnesota Psychological Association (N=708) on March 10, 2015 through Survey Monkey. Because some members reported that they had not received the survey, a web link was established and distributed to members as well. Reminders to complete the survey were emailed on March 16 and 20, and the survey closed on March 22.
A total of 238 responses were received. Of those, 16 were eliminated due to failure to complete the survey, and 6 were eliminated because respondents indicated that they were not members of MPA. This left 216 completed surveys for analysis (response rate of 30.2% of MPA membership at the time of the survey).
Scoring
The 19-item EHR Attitude Scale contained items phrased both in support of and in opposition to the use of EHR. Items phrased in support of the use of EHR were scored in that responses indicating disagreement with the item were scored 1, and responses indicating agreement were scored 4 (Strongly Agree=4, Agree=3, Disagree=2, Strongly Disagree=1). Items phrased in opposition to the use of EHR were scored in the reverse direction (Strongly Disagree=4, Disagree=3, Agree=2, Strongly Agree=1). With this scoring, the closer an item score is to 4, the more the response suggests support of the use of EHR, and conversely, the closer the item score is to 1, the more the response suggests opposition to the use of EHR.
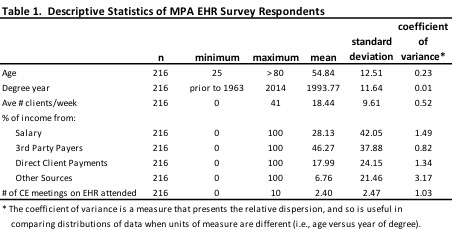
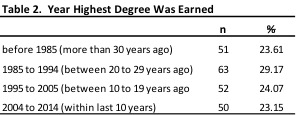
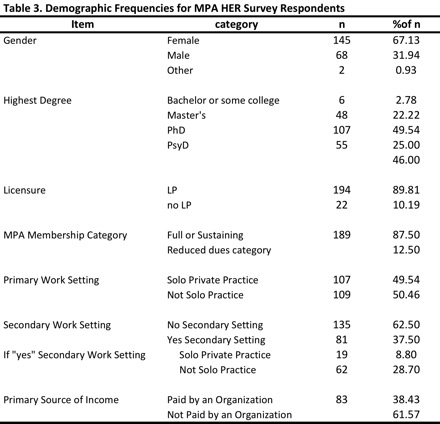
Respondent Demographics
Demographics describing respondents are presented in Tables 1, 2, 3 and 4. The average age of respondents was 55 (range: 25 to >80; SD=12.5). More women than men responded to the survey, which is similar to the proportion of men versus women who are psychologists across the country (Willyard, 2011). Six respondents either had completed undergraduate degrees or some college coursework. Of the remaining respondents, half had completed a PhD, one-fourth had completed a PsyD, and the remainder had completed master’s degrees. The mean year of completing the respondent’s highest degree was 1994 (range: 1963 to 2014; SD=11.6). Note, the lower bound included “prior to 1963” so the scale may slightly over-estimate the average degree year and underestimate the standard deviation. Interestingly, when looking at how many respondents had completed their highest degree within the past 10 years, past 20 years, etc., the spread was almost perfectly allocated into quartiles (see Table 2).
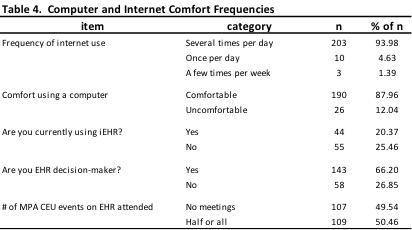
The majority of respondents were Licensed Psychologists, frequent users of the internet, and were the primary decision-makers in the adoption of an EHR product.
On average, respondents reported that they see 18 clients per week (range: 0 to 41; SD=9.6). About half of the respondents reported working in private practice settings, and the other half reported working in group settings, including group private practice, community mental health, medical clinics or hospitals, or academic/research settings. The source of income reported by respondents was primarily from 3rd party payers (46%), followed by salaries (28%), and an average of 18% of respondents’ income was reported as coming directly from client payments.
Among respondents, 86% reported that they were either “Full” or “Sustaining” members of MPA, compared to 69% of MPA members who actually are full or sustaining members. On average respondents reported attending 2.5 CEU sessions on the topic of EHR (range: 0 to 10; SD=2.5). About half of the respondents reported either attending no CEU events at all on the topic of EHR, or attended no CEU events hosted by MPA. The other half reported that at least half or all of the CEU events they attended on the topic of EHR were hosted by MPA.
Notably, there was relatively large variance in how much a respondent’s income came from “salary,” “direct client payments,” and “other sources” which may reflect the diversity of settings in which members are employed. There was also comparatively wide variation in the number of CE units earned by seeking education and training on the topic of EHR (see coefficient of variance column in Table 1).
After obtaining demographic information, the EHR survey offered six items eliciting global ratings of the respondent’s approval or disapproval of EHR in general. Respondents rated their attitude toward EHR as “Very Positive,” “Positive,” “Negative,” or “Very Negative” on the first two items, which were collapsed into two options: “Positive” and “Negative.” On the remaining four items, the response options were “Strongly Agree,” “Agree,” “Disagree,” or “Strongly Disagree,” which also were collapsed into two options: “Agree” and “Disagree.”
Responses to the first two of these six questions are shown in Figure 1 below. Interestingly, respondents tended to be very supportive of the use of EHR in medical settings, with 84% of respondents indicating a positive attitude. In behavioral health settings, however, there was much less agreement, with 44% of respondents indicating a positive attitude toward EHR and 56% indicating a negative attitude toward EHR. Figure 1 presents a visual representation of these differences.
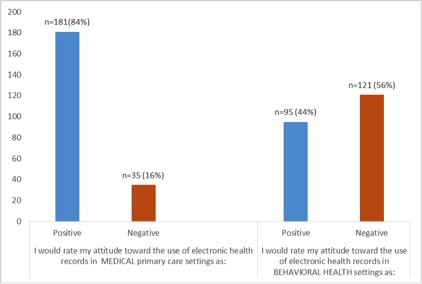
Figure 1. Attitude toward EHR in different healthcare settings
The remaining four global EHR rating items allowed greater refinement in responses by offering the option to respond with N/A indicating that a response was not applicable in the respondent’s case. These can be seen in Table 5. The intention to include “N/A” as a possible response reflected the awareness that some members of MPA do not practice in healthcare settings, and therefore may not be using EHR. However, because respondents were given the chance to opt out from giving global ratings, including these Global EHR items in later analyses led to a decreasing sample size due to missing data.
Among respondents to this survey, two-thirds indicated that they would prefer to opt out of using an EHR in their practice. About 15% of respondents who indicated that they would prefer to opt out of EHR either anticipate that their experience with EHR will be positive, or they chose not to answer this question. Just over half of the respondents predict that clients will object to the use of an EHR. And finally, the Global EHR rating item with the greatest agreement among respondents was the item indicating that respondents would support letting clients determine whether to have behavioral health records to become part of their overall electronic medical record (Agree: n=153, 70.83%; Disagree: n=44; 20.37%).

Analysis
While the simple majority of respondents indicated a negative opinion of EHR, there is by no means a consensus such as is evident in opinions about EHR for medical practice. Far from it, the respondents appear more evenly split in global opinion ratings of EHR in behavioral health settings. Because of the bifurcation of opinion that is evident in Figure 1 above on the question of EHR for behavioral health settings, a cluster analysis was run on the EHR attitude scale items to learn more about the specific reasons for support or dissent by looking at what kinds of possible subgroups exist within MPA members that might partially explain the bifurcation of opinion.
Cluster analysis is a method that attempts to understand the structure of data by placing people in disparate groups based on the statistical properties of their response patterns. The procedure used SPSS two-step cluster analysis. The final number of clusters was allowed to be determined by the algorithm itself rather than user-defined clusters. Using this method, two distinct clusters emerged. The largest cluster (n=131; 60.6%) had responses on the EHR Attitude Scale suggesting that they were more likely to oppose the use of EHR. The smaller cluster (n=85; 39.4%) was characterized by responses on the EHR attitude scale suggesting that respondents were more likely to support the use of EHR. This is consistent with the general breakdown of global ratings in Figure 1.
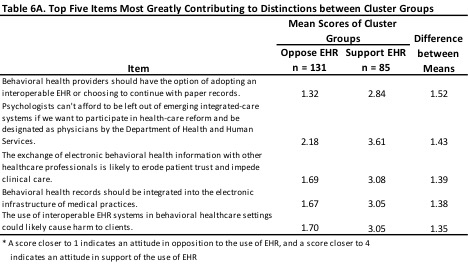
What specifically makes the two clusters attitudinally different? This is where the concrete items offer a more nuanced guide to understanding than a simple yea or nay vote. The mean scores for each cluster on the top five items is shown in Table 6A. These are the items which most greatly polarize the two cluster groups from each other in a statistical sense. For convenience, the clusters are labeled “Oppose EHR” and “Support EHR.” Also for convenience, items were coded so that a low number indicates opposition to EHR while a higher number indicates support. The table indicates, for example, that respondents in the “Oppose EHR” Cluster were more likely to support behavioral health providers having the option of adopting an interoperable EHR or choosing to continue using paper records, while respondents in the “Support EHR” Cluster were more likely to disagree with making the use of interoperable EHR a choice. In essence, the two cluster groups disagree about whether the use of EHR should be optional, whether such use would be harmful, and whether psychologists should be designated as physicians for Medicare.
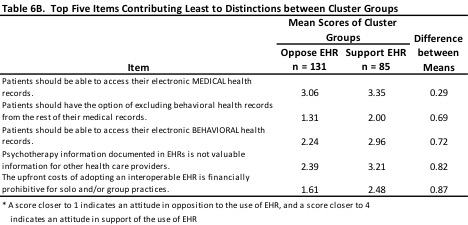
On the other hand, the items upon which respondents in the two cluster groups approach agreement compared to the other items in the scale (see Table 6B) suggest that respondents in the two groups are in greater agreement about patient access to EHR in both medical and behavioral health settings, the value of behavioral health information in medical settings, and the cost of EHR.
Cluster Demographics
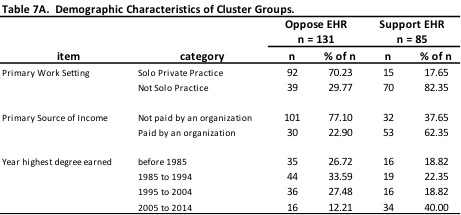
Table 7A provides a few demographic characteristics of the two cluster groups. Respondents in the Oppose EHR cluster tend to work primarily in solo private practice, earn their income from sources other than an organization (directly from third party payers and clients), and have completed their highest degree more than 10 years ago. Respondents in the Support EHR cluster tend to work primarily in group settings (group private practice, community mental health, medical settings, academic settings), are more likely to earn a salary paid by an organization, and are more likely to have completed their highest degree within the last 10 years. Chi-square analysis was run on each of these demographic variables, and all were found to be significant (Asymp Sig>.00001 for each demographic category).
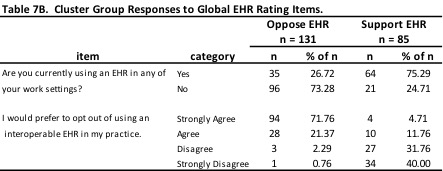
Two additional variables were selected to increase understanding of the cluster groups (see Table 7B). Respondents in the Oppose EHR cluster tended not to be using EHR at the time of taking the survey (n=96; 73%), and indicated that they would prefer to opt out of using an interoperable EHR in their practices (n=122; 93%). Conversely, respondents in the support EHR cluster were more likely to report currently using an EHR in their practice (n=64; 75%), and indicated that they would not prefer to opt out of using an EHR (n=61; 72%). Chi-square analysis was run on each of these global rating variables, and both were found to be significant (Asymp Sig>.00001 for each variable).
Factor Analysis
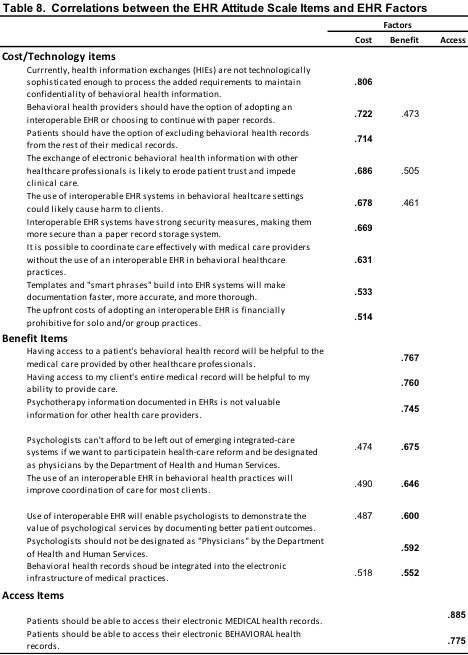
The structural validity of the 19-item EHR Attitude items was measured using exploratory factor analysis. This procedure frequently is used to determine the number of underlying dimensions that explain a group of items, and how strongly each item is linked to the dimension. The extraction method in SPSS Factor Analysis was principal-components, and the rotation method was varimax with Kaiser Normalization.
The rotation converged in five rotations, indicating three underlying factors (see Table 8). The items with the highest loadings on each factor were interpreted semantically to give each factor a meaningful label. It appears that the following labels describe the semantics of the three item groups corresponding to the three derived factors: Cost/Technology, Benefit, and Access. The Cost/Technology Factor contains nine items related to attitudes about technology issues and the cost of using EHR for both providers and patients. The Benefit Factor contains eight items related to attitudes about benefits that may or may not derive from the use of EHR. Only two items loaded on the Access Factor, and both of them are related to attitudes about whether patients should be able to access the EHR.
Discussion
Because members of MPA were asking our organization to formulate a position statement on the use of electronic health records in Minnesota, particularly on whether the largest organization of psychologists in Minnesota was in support of the EHR Mandate or in opposition to it, MPA leadership surveyed members. Our hope was that we would find a collective voice on the issues presented by the Minnesota EHR Mandate. What we found instead is that there is not one voice, but many voices holding many diverse opinions on the use of EHR in Minnesota. We found that psychologists who currently are using EHR, in general find that use valuable. We found that psychologists in private practice, particularly solo private practice, are leery of the use of EHR, and strongly dislike the forced choice that the 2015 Mandate presented. We found that psychologists who are early in their careers are more open to the use and benefits of EHR than are those who have been in practice for decades. We also found that psychologists who are invested in becoming recognized as “physicians” by the Department of Health and Human Services are more supportive of the use of EHR.
In addition to the differences in psychologist attitudes, we found shared areas of concern among psychologists in Minnesota regarding the use of EHR. We found that psychologists shared concerns about the impact of the use of EHR on issues of confidentiality and privacy. We found that psychologists in Minnesota are in agreement that patients should be able to maintain control of their private behavioral health information, and that patients should have access to both their medical and behavioral health records. And finally, we found that psychologists believe that behavioral health information is valuable in overall medical care.
There likely are many more issues that could be highlighted in this discussion, and we encourage everyone to continue the conversation. The coming years ahead of us are presenting rapid and radical change in the practice of psychology. It is vitally important that all of us work together to advocate for the value that psychologists bring to medical care and to people’s lives. The voice of MPA contains diversity, and that diversity is something to be valued and celebrated even when it is a diversity of opinion. It is through the debates that are generated because of disagreement that workable and sustainable solutions can be discovered. And, it is in respectfully engaging with colleagues with whom we disagree that we all work toward protecting our patients as well as our practices. Let us all work together even as we disagree so that Minnesotans can continue to access world class behavioral health care.
Robin McLeod, Ph.D., L.P., is the 2015 MPA President-Elect. She founded and owns a small private practice behavioral health specialty clinic with two locations: Woodbury & St. Paul. You may email her at [email protected]. Her websites are: http://www.cpwmn.com and http://www.cpspmn.com.




